A new smartphone application in development now may soon take the guesswork out of diagnosing jaundice in newborns. It’s called Bilicam, deriving its name from bilirubin, the yellow-colored compound that collects in the baby’s bloodstream while the baby’s liver struggles to filter it out.
Using the Bilicam is simple, as its developers at the University of Washington in Seattle explained in September at the International Joint Conference on Pervasive and Ubiquitous Computing in Seattle, Wash. Parents or health care workers in the field start by placing a strip of paper the size of a business card on the baby’s chest. Then the user points the camera at the baby and the app takes pictures with and without the flash. The paper strip, printed with colored squares, calibrates the camera and accounts for lighting conditions. The app then taps software based in the cloud to judge the presence and severity of jaundice.
“It’s obvious that these kinds of disruptions in the healthcare space have global, not national, implications and opportunity for patients and their families,” Dr. Wendy Sue Swanson, a pediatrician and Executive Director of Digital Health at Seattle Children’s Hospital, who is familiar with the app but not involved in its development, told E4C.
“Digital health tools like this really are hacking health care, taking typically laborious and time-consuming lab draws and potentially facilitating the opportunity for real-time data during clinic or hospital visits. I see it this way: Instead of ordering a lab and waiting six hours for a result, a pediatrician, family doc, or nurse practitioner could get data on the baby’s bilirubin level while at the bedside and be able to make decisions with families at the time of a visit,” Dr. Swanson says.

A common condition
Jaundice afflicts about 60 percent of infants within their first week of birth, according to the US Centers for Disease Control and Prevention. Some of those cases become severe and require medical treatment. Left untreated, severe jaundice can lead to kernicterus, a kind of brain damage that can cause cerebral palsy, hearing and vision loss and mental disability.
Jaundice is one of the most common conditions to afflict newborns and it is also deceptively hard to diagnose. You’ve probably heard that a jaundiced baby’s skin and eyes take on a yellow tinge, but while noticing the change in skin tone might be easy, assessing the severity of the disease through a visual inspection can be difficult, even for the experts. When doctors compare their visual assessment to blood tests, their diagnoses fall within a broad range from pretty accurate to not even close, studies have found.
How accurate is the Bilicam?
Compared to a visual assessment, the Bilicam may already be much more accurate, and it may yet improve with further development.
It even comes close to the accuracy of a blood test. Blood tests must be performed in a medical lab and they are considered the gold standard of jaundice diagnosis. In a recent trial with 100 newborns, Bilicam scored a .85 rank order correlation coefficient compared to the blood test. On that scale, a 1 would be a seamless match between the two methods with no differences in their results, and a 0 would suggest no match at all between the two.
With improvement, the app could soon compete with a much more expensive diagnostic device, the transcutaneous bilirubinometer, says Dr. Jim Taylor, a pediatrician at the University of Seattle, who is helping to develop the technology.
The transcutaneous bilirubinometer is a hand-held instrument that estimates bilirubin levels using light pulses bounced against the newborn’s skin. Each device costs several thousand dollars and they are used most often in hospitals. It correlates to the blood test in a coefficient range of .75 to .93, the latest trial found.
Design challenges
A few development obstacles lie ahead for the Bilicam team says Lilian de Greef, a doctoral student in computer science and engineering at the University of Washington who is involved in developing the technology.
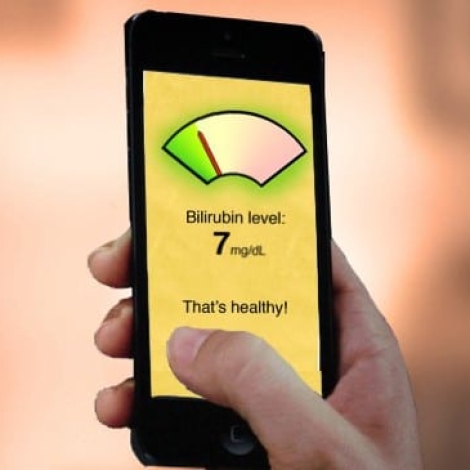
“There are a number of aspects we want to improve. One of them is the card. We have some new designs in mind to make the whole process smoother and more accurate, including features such as a slot to frame the patch of skin we’re interested in. At some point we’ll also need to investigate how to best frame the sample-collection process and how to display results for end users. Currently, everything we developed was mostly to collect data and process them for our evaluation. There’s still lots of work to be done on how to present everything for users like parents,” de Greef says.
One advantage to storing the software in the cloud is that the Bilicam team can continuously improve the algorythms that Bilicam uses to analyze skin tones and other aspects of the diagnosis, even after the app is released.
A phased rollout
Dr. Taylor didn’t give an exact timeline for Bilicam’s release, but the team plans to offer it in phases. The first adopters will be clinicians who can interpret the results, then it will be offered to parents.
Cheaper, greener jaundice treatment
Machines built in recent years have shown us that treating jaundice, and now diagnosing it, does not have to be expensive. The condition is commonly treated with phototherapy by bathing the infant in blue light calibrated to shine within a certain frequency. The light breaks down the bilirubin in the blood. Conventional phototherapy machines cost thousands of dollars and gorge on electricity, making them inaccessible to clinics with poor funding and intermittent power supplies. Design Revolution in San Francisco has responded with Brilliance, a phototherapy machine that costs less and consumes less power than traditional machines. We report on it here: Cheaper, greener blue light: A better phototherapy device for jaundice treatment.