Using paper, a couple of assays and a simple foam stamp, a new manufacturing technique can make disease screening strips more affordable.
Treatable diseases often go undetected in developing countries due to the high cost and scarcity of screening technology. Many treatable diseases, like diabetes and urinary tract infections, can be detected via urinalysis, or analysis of urine. While urinalysis test strips are commonly used in developed countries, they are less practical for developing countries because they require high capital and import costs, complex manufacturing systems, and intricate supply chains.
Changing the Way We Look at Test Strip Manufacturing
Commonly used test strips can be broken down into three components: a substrate, an assay (where we see a color change), and an applicator (an instrument that applies the assay to the substrate). Test strips made via conventional manufacturing processes use a multi-layer substrate containing plastic, absorbent pads, meshes, and a series of assays used to detect different disease markers, as shown in the image below. The manufacturing process itself requires a large and intricate assembly line involving rollers, cutters, chemical brewers, and applicators, among other pieces of machinery. So, how can we simplify the manufacturing process to make it more appropriate for developing countries?
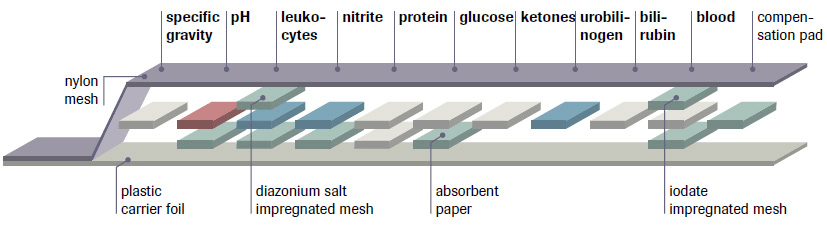
Cross-section of urine test strip created by conventional manufacturing (Source: Roche Diagnostics USA)
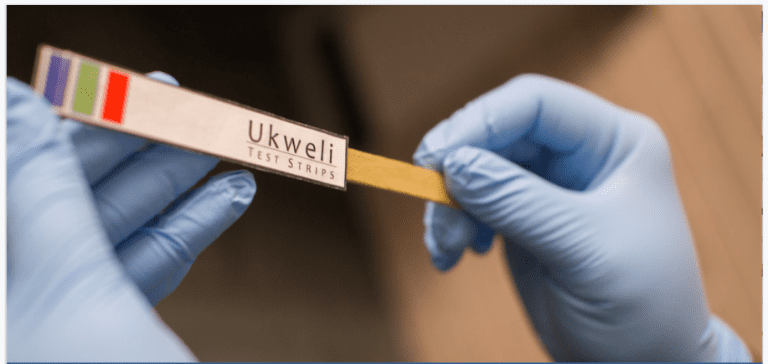
The Humanitarian Engineering and Social Entrepreneurship (HESE) Program at Penn State University is exploring an alternative approach: creating an affordable point-of-care urinalysis screening tool that can be manufactured using paper, a couple of assays, and a simple foam stamp, as shown below. This approach simplifies a traditionally complex system by replacing the multi-layer substrate with filter paper and by replacing the manufacturing assembly with an operator and a foam stamp.
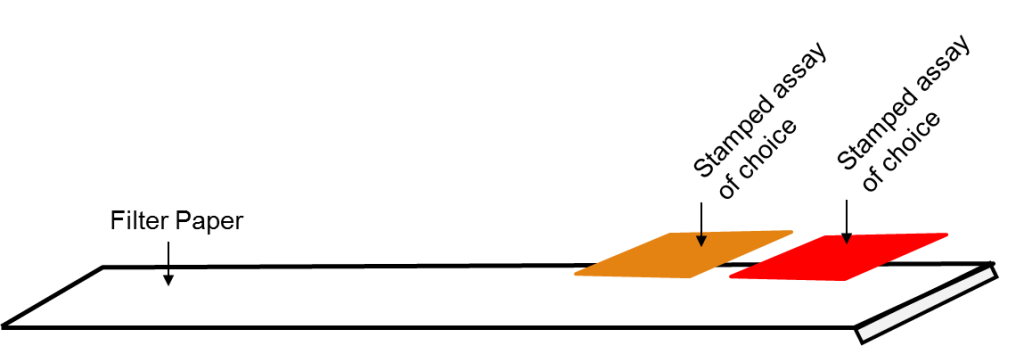
This image shows a cross-section of urine test strip created by stamping. Each assay can screen for one marker (e.g., nitrite, glucose, bilirubin, etc.). As a result, stamped test strips can be customized to screen for particular diseases based on the selection of assays. For example, a test strip that screens for diabetes will contain a glucose assay and a ketones assay. Through this method of manufacturing, we develop a system that is affordable, accessible, and tailored to be sustainable in resource-constrained areas.
Shifting from Printing to Stamping
Our team previously explored a manufacturing approach that repurposed an inkjet printer by filling empty ink cartridges with assays. The printer “printed” the assays onto paper, which could then be cut into test strips. Further investigation, however, showed that printing was not suitable for resource-constrained contexts due to an unreliable electricity supply, mechanical issues, and relatively high expense. As a result, we turned to stamping: a method in which we dipped a common store-bought stamp into an assay and pressed it onto a substrate.
In a study exploring the use of stamping for test strip manufacturing, we tested many low-cost and widely available substrates (e.g., printer paper, cardstock, paper towel, etc.). We chose filter paper as an appropriate substrate because it was durable, assay-friendly, and reduced substrate costs to approximately 3 cents (USD) per strip. We also tested many different applicators (e.g., rubber stamps, self-inking stamps, droppers, etc.), but chose a foam stamp because it was low-cost, durable, and produced consistent results. Using the stamping method described, our team was able to successfully create urinalysis test strips that screen for diabetes markers.
Making a Case for Stamping
The beauty and merit of the stamping method is that it decomposes the complexity of conventional test-strip manufacturing to its bare minimum: a low-cost, widely available substrate, an assay, and a foam stamp for easy assay application. In turn, the stamping method can be integrated into any setting with minimum startup cost (less than $10 USD). More so, it tackles the three main barriers (affordability, availability, and accessibility) to preemptive disease screening in developing countries.
Commonly used test strips cost 5 to 15 cents to manufacture, depending on the number of assays. In comparison, stamped test strips cost 2 to 10 cents to manufacture, thus creating a more affordable disease screening device.
In terms of availability, the stamping method enables quick turnover because it takes a matter of seconds to stamp each test strip. As a result, test strips can be manufactured in a “made to order” fashion depending on the flow and demand of customers.
Because the stamping method does not require heavy machinery or significant technical expertise, test strips can be manufactured in both urban and rural settings, giving individuals in remote communities access to valuable and potentially life-saving disease screening technology.
Looking Ahead: Challenges & Scalability
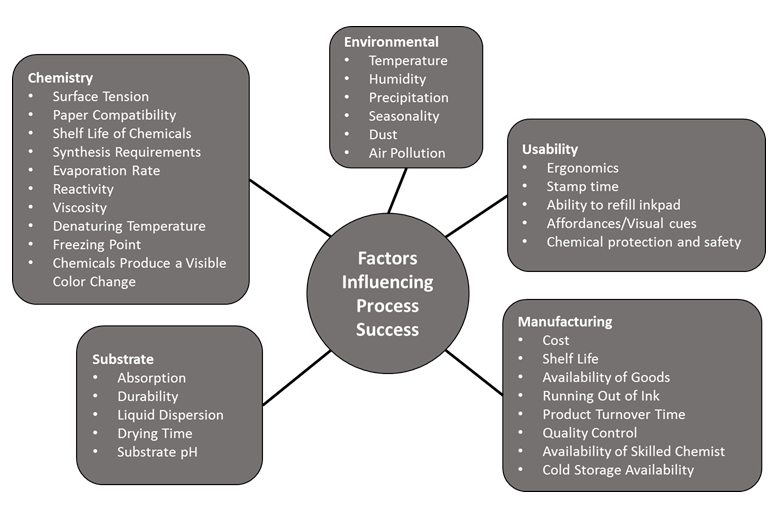
While initial tests to develop diabetes screening strips via stamping show promising results, many challenges remain in marketing and establishing a new manufacturing process outlined in the chart below. One factor that influences manufacturing success is the assay component, which has precise protocols and environmental and storage requirements. Other challenges involve the shelf life of stamped strips, quality control, environmental controls, and training individuals on how to make and use the strips.
In the upcoming years, our goal is to formally validate stamping as a reliable manufacturing method to create affordable, easily available, and easily accessible screening test strips. Looking forward to scaling opportunities, the proposed stamping mechanism can be customized to screen for different conditions (e.g., diabetes, urinary tract infections, water purity, pregnancy, and methanol levels in alcohol) by simply swapping assays. Ultimately, this stamping method has wide scope for humanitarian engineering applications in the fields of healthcare and environmental safety.
Further Reading
- G. Gundermann, S. Sen, S. Ritter, K. Mehta, “Stamping: A Low Cost Manufacturing Method To Stamp Assays.” in 2016 IEEE Global Humanitarian Technology Conference.
- Arnett, A. Winkler, A. Vergani, S. Ritter, K. Mehta, “Inexpensive urinalysis test strips to screen for diabetes in developing countries.” in 2016 IEEE Global Humanitarian Technology Conference.
Shweta Sen, Sarah Ritter and Gabrielle Gundermann are in the Humanitarian Engineering and Social Entrepreneurship (HESE) Program at Pennsylvania State University, and Khanjan Mehta is the program’s founding director.