A new large-scale trial of clean-burning rocket stoves and water filters in the poorest households in Western Province, Rwanda, adds evidence supporting their efficacy in improving respiratory and digestive health. But the findings hint at potential uptake obstacles, according to a study published June 3 in PLOS Medicine.
In a cluster-randomized controlled trial, researchers at the London School of Hygiene and Tropical Medicine (UK) and Emory University in Atlanta, Georgia (USA), examined health outcomes of children under five years old in nearly 1600 households, half of which had received filters and stoves. The devices were linked to a 29 percent reduction in diarrhea and 25 percent reduction in acute respiratory infections.
“These results have important implications for the viability of promoting and sustaining household health interventions at scale. This program and study are among the largest ever conducted of these kinds of interventions,” Evan Thomas, director of the Mortenson Center for Global Engineering at the University of Colorado, Boulder, said by email.
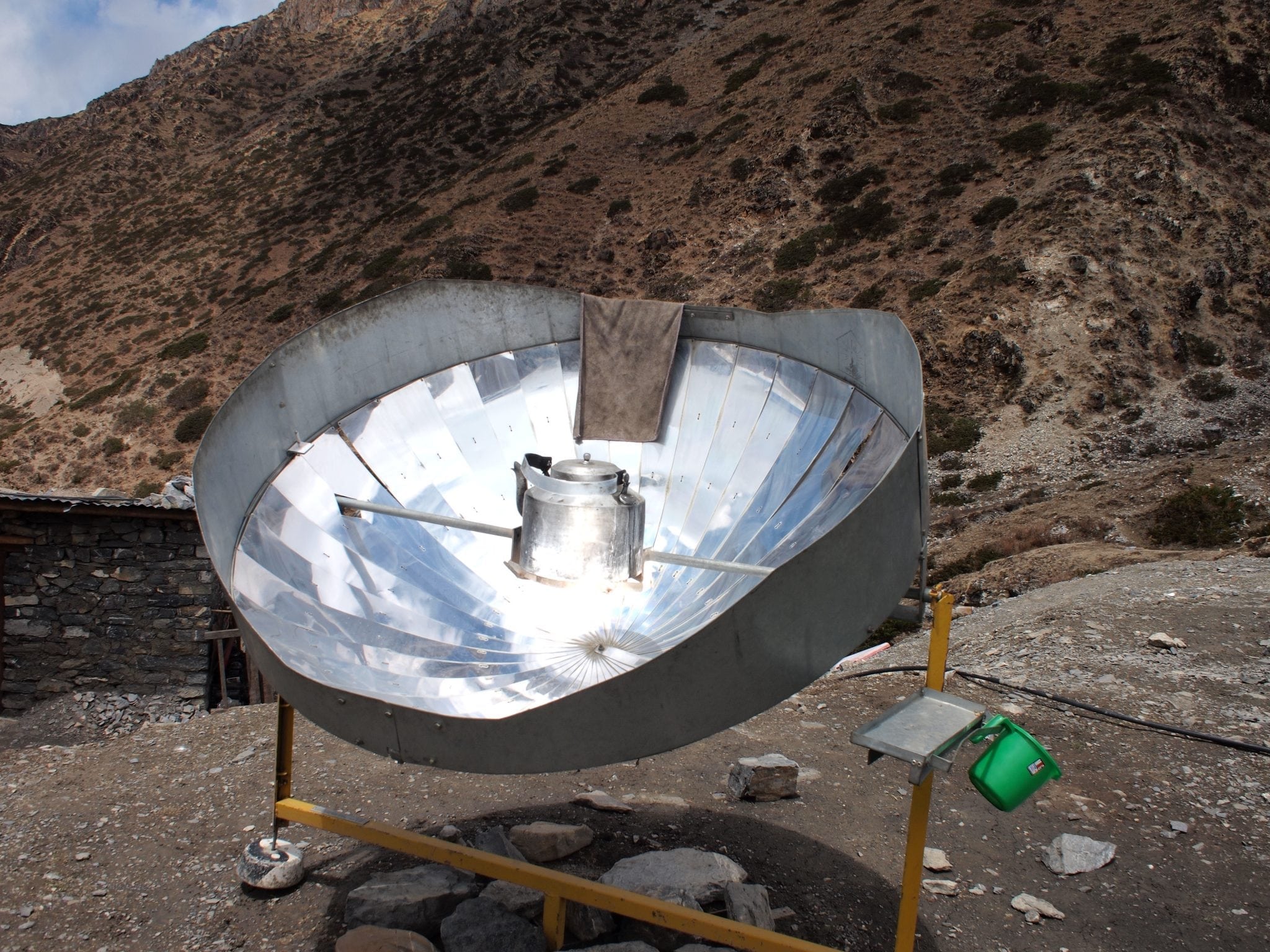
Since 2003, Dr. Thomas has been instrumental in the stove and filter distribution program that was the subject of the study. From 2012-2016, Dr. Thomas directed a $25 million push to scale up the intervention, working as Chief Operating Officer at the social enterprise DelAgua Health. The program partnered with Rwanda’s Ministry of Health to deliver filters and stoves to nearly half a million people in 2014, and delivered stoves to another 1.2 million people from 2015-2016.
Before the trial began, 76 percent of the households studied drew drinking water from an improved source such as pipes, boreholes, protected springs and wells, and rainwater. And more than 99 percent cooked on traditional (not improved) biomass-burning stoves. Follow up over the course of roughly one year found that about two-thirds of the households reported using their water filters every day, and usage of both stoves and filters decreased over time.
“After neonatal disorders, pneumonia and diarrheal disease are the two leading killers of children under five years of age in Rwanda and much of sub-Saharan Africa,” the study’s lead author Thomas Clasen, faculty at Emory University and the London School of Hygiene and Tropical Medicine, said in a statement.
“The results of this randomized controlled trial provide strong evidence that effective interventions can be successfully delivered and embraced by a population at risk, even in remote rural settings,” Dr. Clasen says.
An important aspect of this study is the quantity and quality of data available. Rather than relying solely on the word of the people in the trial to describe how they use the new technology, this trial included stove usage and indoor air quality monitors to provide quantifiable data. DelAgua Health has focused part of its R&D budget on developing such sensors. Harvard Personal Exposure Monitors worn by cooks found that cooking with improved stoves had no significant effect on exposure to fine-particulate matter (PM 2.5).
Past studies that yielded mixed results of indoor air quality in kitchens with clean cookstoves have suggested that the lack of improvement may stem from “stove stacking,” in which cooks use their traditional smoky stoves alongside the improved stoves. This new study also mentions that PM2.5 measurement was limited, suggesting that the results may not reflect the experience of most people over time.
Read more about sensing devices in Evan Thomas’ article, The Internet of Broken Things
Future research may look into other potential impacts of water filters and rocket stoves, such as time saved and other types of disease avoided, the researchers wrote.
Read the study in PLOS Medicine: Effects of a large-scale distribution of water filters and natural draft rocket-style cookstoves on diarrhea and acute respiratory infection: A cluster-randomized controlled trial in Western Province, Rwanda